How to Treat Patients with ARFID via Telehealth
Abridged transcript and slides
Presented by Dr. Jennifer Thomas (Massachusetts General Hospital) and Elissa Martinez LMFT (Recovery Record)
Access to the full webinar recording and all the slides are availabel from IAEDP.
Pages: 1 2 3 4 5 6 7 8 9 10 11
Agenda
Elissa and I are really excited to talk to you about treating ARFID via telehealth. This is Jenny Thomas, starting, and Elissa will go next. But I wanted to just start off with some disclosures. I do receive royalties for the sale of my books and a few other income streams. I think most notably probably related to this presentation is that I do get some royalties for my two books that are about ARFID.
There are really three topics that Elissa and I wanted to present to you. The first thing that we wanted to talk about is first of all just how is ARFID assessed. So if you have a patient coming into your practice, how will you know if they have ARFID, how will you know what type of features they might have and what should be targeted in the treatment, and how will you know if they're getting better. The second piece that we wanted to cover is what is CBT-AR or cognitive behavioral therapy for ARFID, which is a treatment that my colleagues and I have developed here at Mass General Hospital. And how can you deliver it via telehealth in this age of the COVID-19 pandemic where a lot of us are not able to do in-person sessions with our patients. And then lastly, and Elissa will really take this part home for us will be, how can digital tools, things like apps like Recovery Records, support CBT-AR delivery.
How is ARFID Assessed
Let's start with, how is our ARFID assessed? Well, if you guys are tuning for a webinar on ARFID, you're probably familiar with the diagnostic criteria, but I'll just review them very briefly. Basically individuals with ARFID have a persistent failure to meet their nutritional needs. They have difficulty eating enough food in terms of either the volumes, so number of calories, or in terms of the variety. So maybe they're not able to eat a wide enough variety of food groups, maybe they only eat one or two foods or food groups total. And it's really above and beyond just regular kind of picky eating or fussy eating because it has to lead to certain consequences. Things like either very precipitous and significant weight loss or difficulty growing taller or gaining weight as expected if it's in children. It can lead to significant nutritional deficiencies and often unusual one.
So we've worked with patients in our clinic who have not just things like low iron or B12, which we see routinely in other eating disorders, but maybe even things like low vitamin K or low vitamin C because they aren't eating enough fruits and vegetables, for example. Many of these patients are dependent on supplements. So either calorie drinks like Ensure or Boost or on vitamin. So maybe they have to get like B12 injections or to take a multivitamin every single day prescribed by a physician. And then lastly, many of these folks also have a lot of psycho-social impairment. We've worked with patients who, for example, can't eat outside of their own home because they're terrified of what food might be like prepared elsewhere. Maybe they can't go on dates or eat in the cafeteria at work or school. So that really gets in their way of them being able to live a full life that they want to live.
Importantly, the selective eating in ARFID, it can't be due to just like food not being available or food insecurity and it can't be accounted for fully by another medical or psychiatric condition, although often those conditions do co-occur. And it can't be due to fear of weight gain or body image disturbance. That's what really makes ARFID kind of a really different presentation to anorexia nervosa or bulimia nervosa or binge eating disorder, for example.
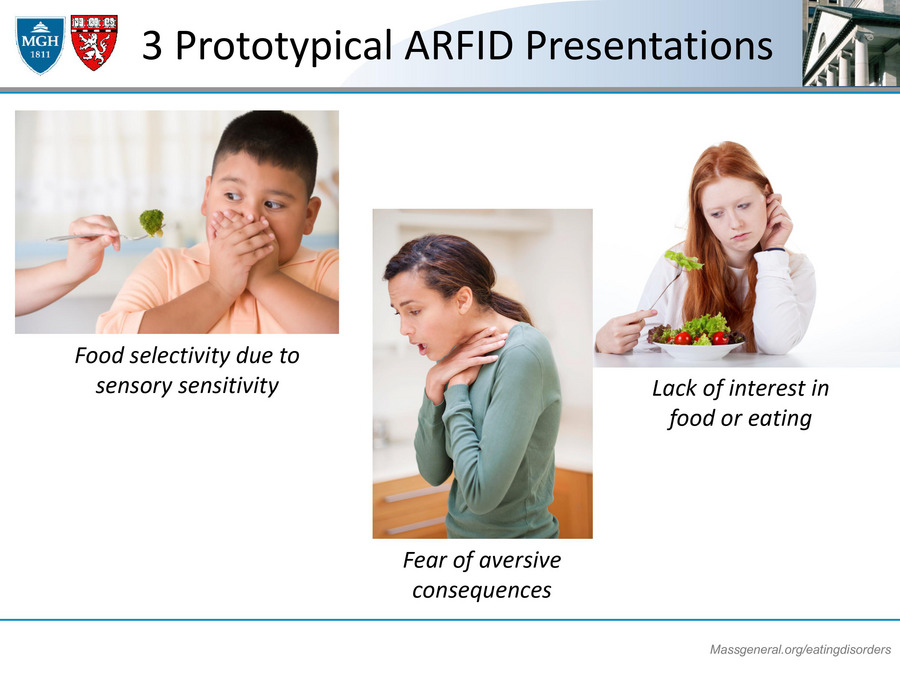
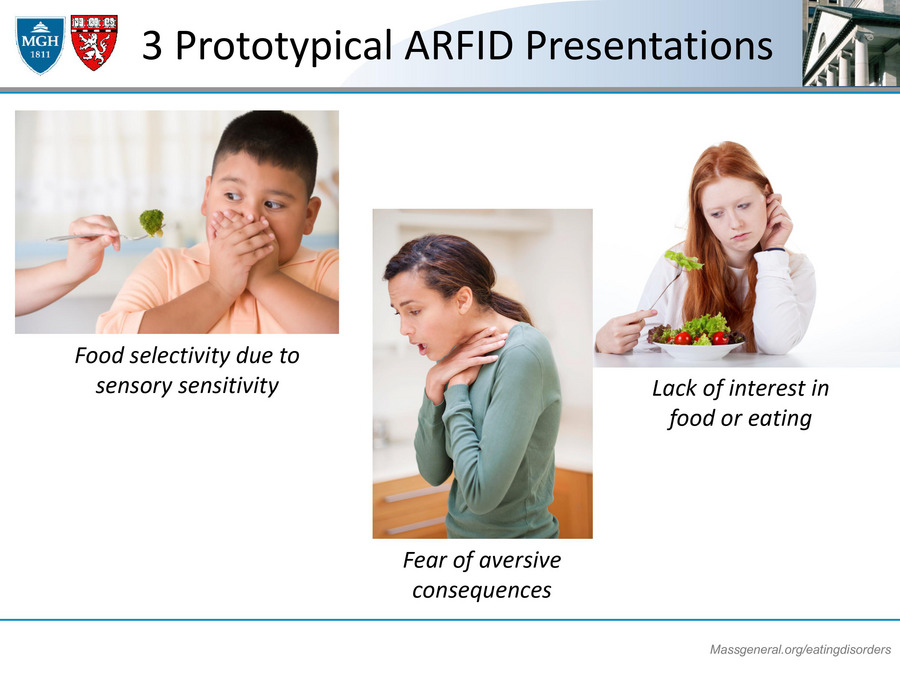
3 Prototypical ARFID Presentations
Now, if folks are not restricting due to concerns about shape and weight, there are really three prototypical presentations of ARFID, really like three reasons why our patients will tell us that they have difficulty eating. The first one is food selectivity due to sensory sensitivity. These would be the patients that say, "Oh gosh, it's just really hard for me to eat broccoli or any vegetables because I'm just worried that they'll taste disgusting or they'll be slimy or they're too crunchy or they won't be the right temperature." These patients really have like a neophobia of trying and taking on board new foods.
We also see patients who have a fear of aversive consequences. They're just really terrified of eating either specific foods or even eating anything at all because they're afraid that the food will make them vomit or choke, or maybe have a lot of belly pain or diarrhea or be in pain, have an allergic reaction. They're afraid that something really bad will happen acutely when they're eating. And then lastly, we also see patients who express a real lack of interest in food or eating. They'll think that eating is a chore. They don't look forward to it and they really don't feel hungry. And I would say this last presentation sometimes can be a little tricky in practice to differentiate from anorexia nervosa because there are a lot of overlapping features there.