How to Treat Patients with ARFID via Telehealth
Abridged transcript and slides
Presented by Dr. Jennifer Thomas (Massachusetts General Hospital) and Elissa Martinez LMFT (Recovery Record)
Access to the full webinar recording and all the slides are availabel from IAEDP.
Pages: 1 2 3 4 5 6 7 8 9 10 11
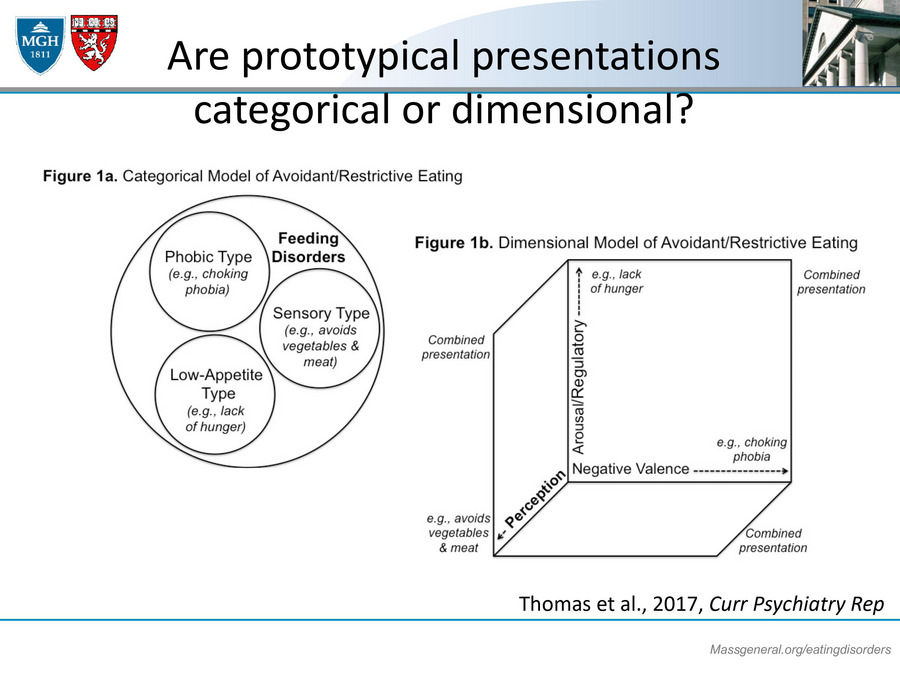
Are prototypical presentations categorical or dimensional?
Now, one of the things that my group has wondered a lot about is whether these presentations are kind of categorical or dimensional. One way of thinking about these presentations would be subtypes that are mutually exclusive. But what we actually tend to see in clinical practice is that patients might come with all three presentations or maybe they'll have two, maybe one is more severe than the other but they have two that are present. For example, one of the very first patients that I saw with ARFID who came to our clinic was a young girl, 11 years old, who had always sort of been a selective eater for her entire life. Didn't really eat very many fruits or vegetables. She always had been fairly glow on the growth curve and homesick for a percentile, never really was that interested in eating.
But the reason she presented acutely is because she had a choking episode on a pork chop and then became afraid of eating pork chops and then afraid of eating all meat and then really afraid of eating anything at all except for liquids. I think when she came in, she was only really drinking milk and Pedialyte. So she was an example of somebody who had all three presentations. And so one of the ways that I like to think about ARFID is that you might be able to sort of plot somebody's symptoms in like a three-dimensional space, like a cube. So sort of the severity of their lack of interest or the severity of their sensory sensitivity or the severity of their fear of aversive consequences and that the presence and severity of each of those phenotypes should really kind of drive what sort of treatment that you might provide.
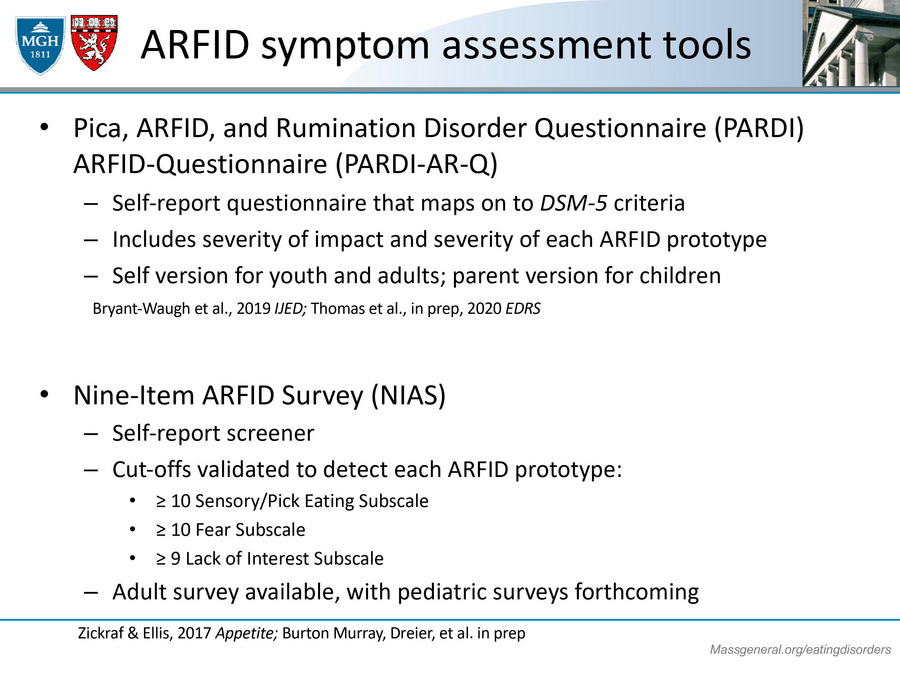
ARFID symptoms and assessment tools
In terms of assessment tools, it's really early days with this ARFID work but there are two tools that I could recommend that you could use in your practice and both of them are freely available. First, there's the Pica, ARFID, and Rumination Disorder interview, which we also have turned into a questionnaire. This is a questionnaire that I've developed in concert with some colleagues: Rachel Bryant-Waugh, Lucy Cooke, Nadia Micali, and Kamryn Eddy. It's a self-report questionnaire that really maps onto those DSM-5 criteria for ARFID that I shared with you and it includes a score for severity of impact. So kind of how bad is the ARFID in terms of the symptoms, how much is it impacting the individual, and it also includes information or items that people can fill out to ascertain the severity of the ARFID prototypes so that you could figure out very quickly from the questionnaire is this somebody who has a fear of aversive consequences or sensory sensitivity or lack of interest.
And importantly, in this questionnaire, we have a version for youth and adults that's kind of a self test. And then we also have a parent version for children who might be responding on behalf of their kids in terms of what they themselves have observed. Another option for a tool, which is also freely available and is very nice. I mean, it's the Nine-Item ARFID screen. Sorry, it's a survey but it's meant to say screen. So the Nine-Item ARFID screen or NIAS, which is developed by Hana Zickgraf and her colleagues, and this is another self-report measure. Right now it's only available for adults, but they're looking in piloting a pediatric version. This one is nice because it has specific cutoffs on each of the sub scales to help you determine, again, what type of ARFID somebody might have, whether it be sort of picky eating, fear or lack of interest. So those would all be really useful, I think, for you to give to a prospective ARFID patient right from the get-go in session one.
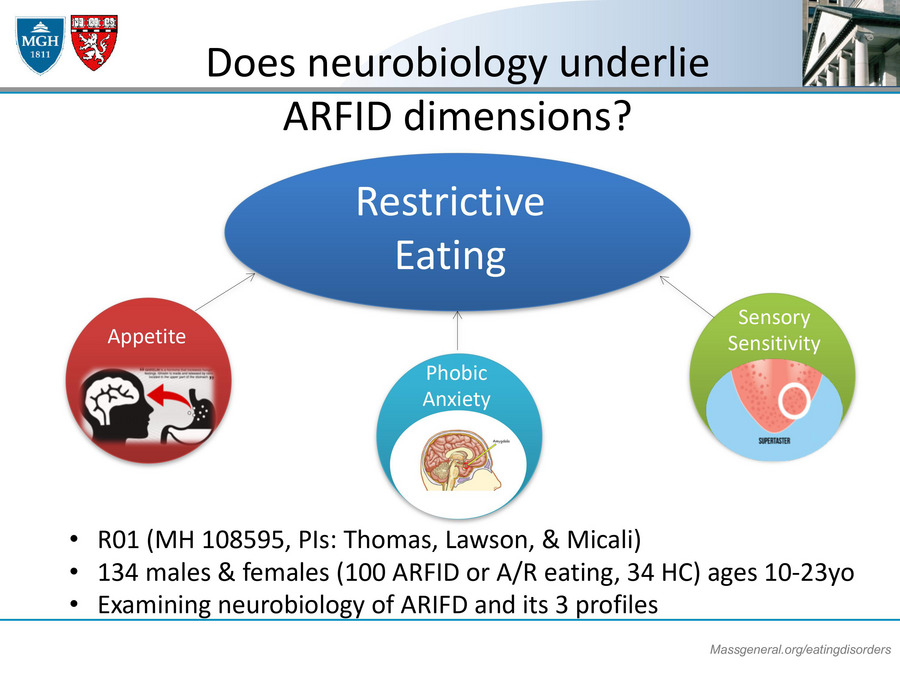
Does neurobiology underline ARFID dimensions?
One of the things I wanted to just share with you before getting into some of the specific treatment interventions is, what do we know about the neurobiology of ARFID? This is an area of great interest to my colleagues and I at Mass General. We really don't think that anyone would choose to have ARFID or really any other eating disorder for that matter. And so what we're doing is trying to figure out if there might be unique neuro-biological profiles, something unique pattern of brain functioning, hormone functioning, other symptoms that might co-occur with the ARFID kind of sensory perception that would help us to determine why somebody might be at risk for ARFID or what may make the ARFID persist. So I'm just going to give you a little bit of a taste to some of the work that our group is doing in this area.