How to Treat Patients with ARFID via Telehealth
Abridged transcript and slides
Presented by Dr. Jennifer Thomas (Massachusetts General Hospital) and Elissa Martinez LMFT (Recovery Record)
Access to the full webinar recording and all the slides are availabel from IAEDP.
Pages: 1 2 3 4 5 6 7 8 9 10 11
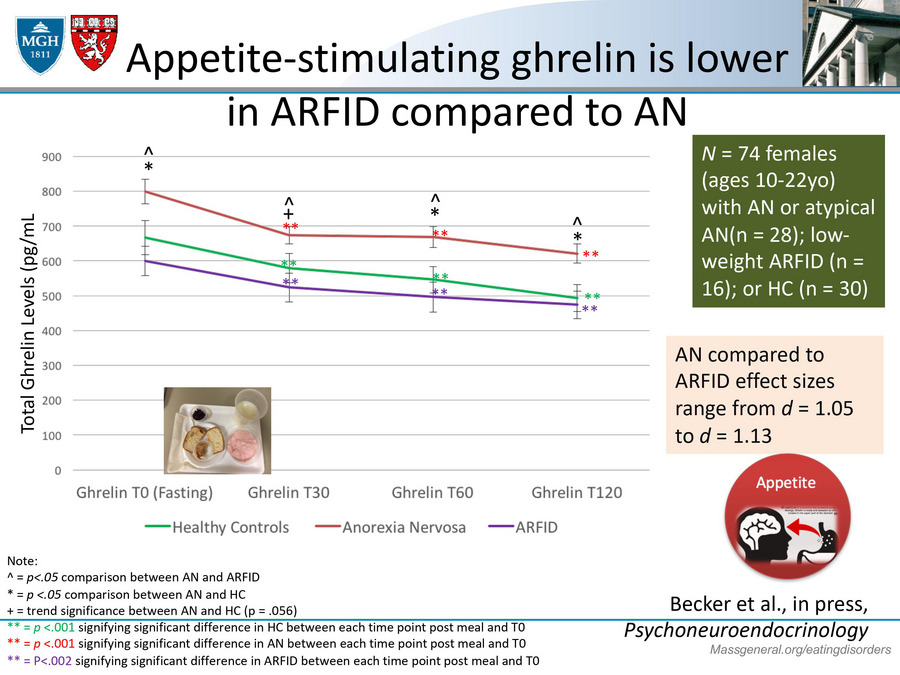
Appetite-stimulating ghrelin is lower in ARFID compared to AN
So specifically with the low appetite phenotype, this is some work from my colleague, Kendra Becker, and we have patients that come into our laboratory who they haven't eaten anything, it's very early in the morning, and then we give them access to a test meal, like I've given this picture here with maybe some toast and yogurt. And one of the things we do is we test for their appetite regulating hormones. And so in this slide, I just want to draw your attention that here we're looking at ghrelin, which is an appetite stimulating hormone. It's a hormone that kind of makes you feel hungry. So after an overnight fast, you would want it to probably be pretty high or ready for breakfast.
And what we actually found is that low weight girls with ARFID represented in the purple line actually had very low levels of ghrelin compared to the healthy individuals and also those with anorexia nervosa who had higher levels. And so that just helped us to kind of empathize that when many of our patients with ARFID are saying, "Look, I just don't feel hungry. It doesn't occur to me to eat." That actually might be partly biologically mediated. We don't know if the low ghrelin is a cause or a consequence of the ARFID, but it certainly might be something that kind of keeps it going.
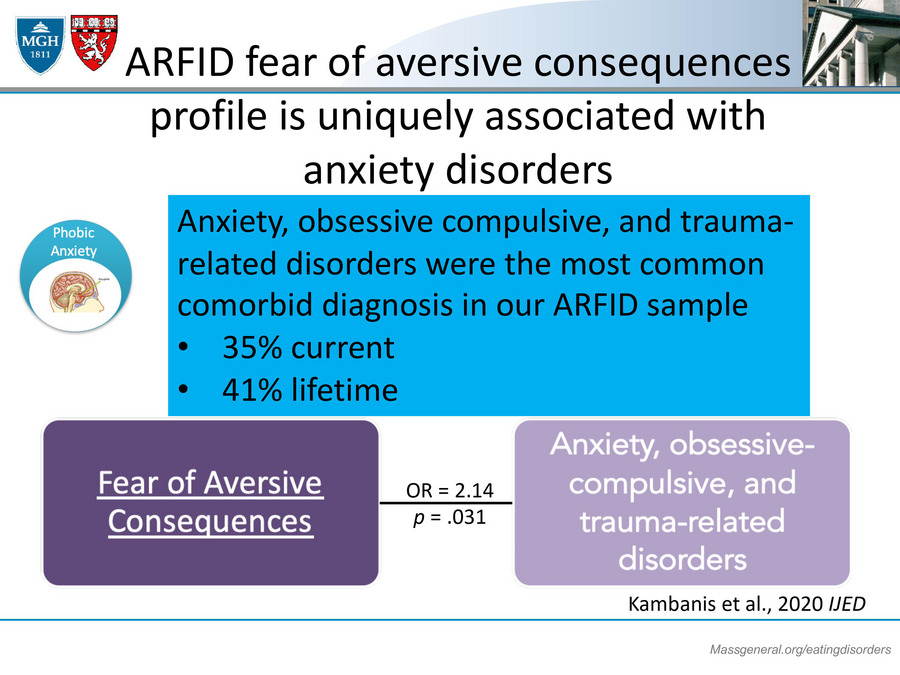
ARFID fear adversion consequences profile is uniquely associated with anxiety disorders
Another thing that we've found is that individuals with ARFID are at a very high risk for anxiety disorders. In our sample of folks with ARFID, a third of them had a current anxiety disorder and 40% had a lifetime anxiety disorder and anxiety disorders were actually particularly relevant for those who have that fear of aversive consequences presentation. I think back to one of my patients who presented with a fear of choking. She also reported that as a very young person, she was afraid of balloons and elevators and clowns and dogs. So really there might be like this high anxiety phenotype that puts people at risk for this particular ARFID presentation.
And then lastly, this is kind of a hot off the press study that one of my postdocs, Stephanie Harshman, is writing up for publication, and this was looking at sensitivity to bitter taste in individuals who have ARFID. And what we actually found is that if you ask folks with ARFID to swish around a solution that is fairly bitter, something is quinine in it, or to have a piece of paper in their mouth, which again is a fairly bitter tasting substance for some people, that they actually rate those experiences as more intense and their rating of their bitterness is more intense compared to healthy controls. That leads us to believe that folks with ARFID may be really kind of exquisitely in tune with the bitterness of foods or the tastes of foods which might make things taste very intense to them and that might be why it's kind of difficult for them to add on board new foods.
ARFID treatments should target these mechanisms
And so really I just bring all of this up to highlight that I think that our food treatment should really target these mechanisms. We need to help people with their lack of hunger. We need to help people with their anxiety. And we need to help people with the fact that they might be a little extra sensitive to trying certain foods for the first time. So that leads me to what is cognitive behavioral therapy for ARFID or CBT-AR, and how can it be delivered through telehealth? Okay. CBT-AR is a flexible modular treatment for children, adolescents, and adults that comprises about 20 sessions over four stages. The stages include psycho-education.