How to Treat Patients with ARFID via Telehealth
Abridged transcript and slides
Presented by Dr. Jennifer Thomas (Massachusetts General Hospital) and Elissa Martinez LMFT (Recovery Record)
Access to the full webinar recording and all the slides are availabel from IAEDP.
Pages: 1 2 3 4 5 6 7 8 9 10 11
Outline of a typical session
Here's an outline of a typical session, which again, we designed this treatment to take place in person but we've been now doing it totally virtually over telehealth and it seems to work just as well. First, we always set the agenda. We like to tell the patient or the family what we'll be going over. We then take the patient's weight, which is particularly important if they're underweight and need to gain weight. We review their homework from the last session except for of course in session one, they haven't had any homework gap but we'll review it in the later sessions.
Then we'll implement whatever the intervention is related to the current treatment stage, and I'll go into more detail on that as we go through, and then we'll review any agenda items that are brought in by the patient in or the significant others. And then lastly, we'll plan some at-home practice tasks to be completed before the next session. And that's pretty important that patients are doing practices and homeworks in between the session because there's only so much you can do in a brief treatment of 20 to 30 sessions. And so the patients will need to do a lot of the work on their own.
Another telehealth tip is that patients will need to have a scale at home in order to do this treatment. I don't usually care whether or not a patient has a scale at home. Sometimes with other eating disorders, it's maybe better that they don't. But in this case, if your patient's not able to come in and see you in the clinic, it is really important that they have their own scale. So whether they need to get that on Amazon or from a friend and so on, that will be really crucial.
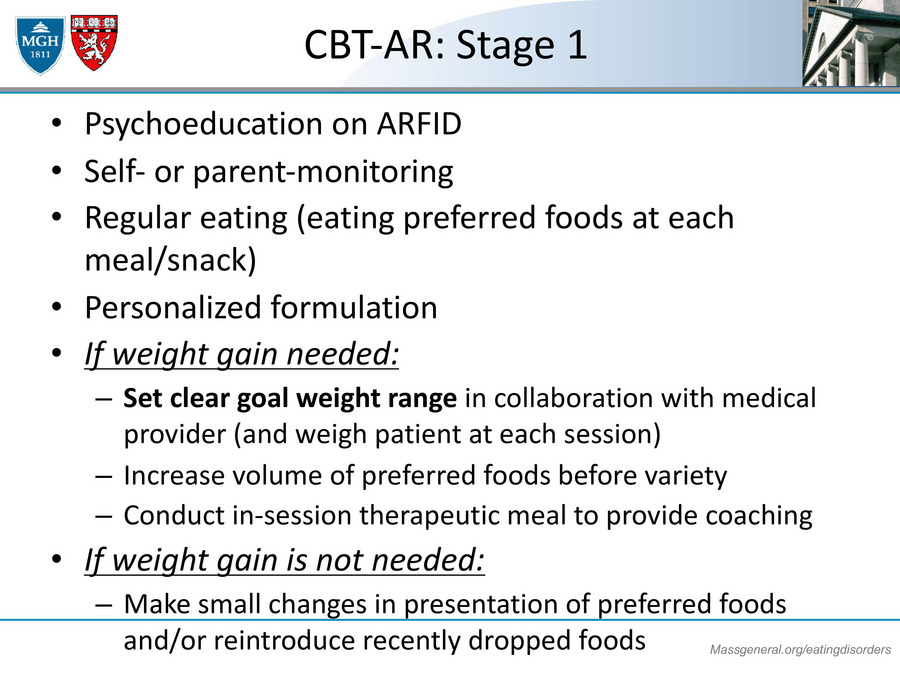
CBT-AR Stage 1
Stage one. The main interventions of stage one of CBT-AR are our first preventing psycho-education on ARFID, kind of in the way that I did at the beginning of the talk. Just letting patients know what the diagnosis is, how do they fit criteria, maybe providing feedback on how they scored on the measures that you gave them. We also ask patients to do some self-monitoring to indicate like what are they eating throughout the day and what feelings might be associated with that, what thoughts. And so that way you can keep track of how are they doing with the homework, are they eating regularly, are they skipping a lot of meals? Are they adding Friday, are they not?
We also encourage patients to work on regular eating. We start with preferred foods because this is our first treatment. So we don't ask them right away like, hey, add a bunch of vegetables or eat all the foods that you're afraid of. But we'll say, "Let's get a nice framework going so that you're having breakfast, lunch, dinner, and one to three snacks depending on if the person needs to gain weight, they'll need to do more. But we want to have a nice framework that then we can hang our hats on later in the treatment in terms of adding variety.
We also work with them on creating a personalized formulation, which I'll show you in a moment. And if the patient gets to gain weight, we will collaborate with their medical provider to help them figure out what the goal range is. And we really encourage them to try to increase their volume of preferred foods, again, before increasing variety. We'll conduct an in-session therapeutic meal to provide coaching. And then if the weight gain is not needed, then we'll actually just have them start making small changes in the presentations of preferred foods, or maybe to reintroduce recently dropped foods. So we don't go on all in right away and increasing variety, but we'll ask them to start with some small changes.
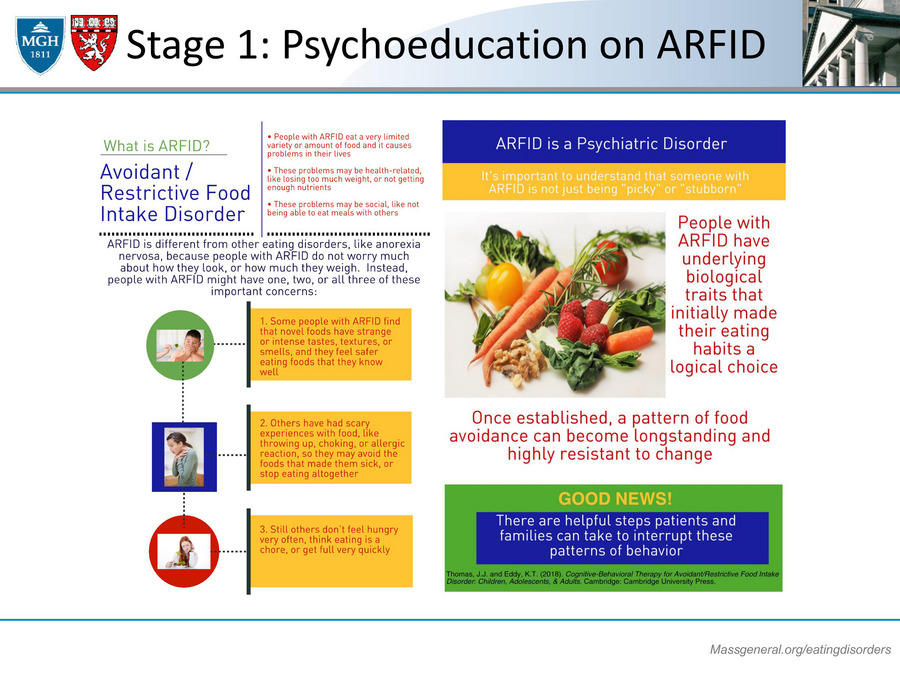
A couple of telehealth tips here is that when we provide psycho-education in the telehealth setting, we'll try to screen-share the handouts, and I'll show you an example of that. Another thing that you can do that's really great and many of you are probably already doing this, but it's to use an app for self-monitoring, and Elissa is going to talk a lot more about that later this afternoon. This is just an example of a psycho-education handout on ARFID that's from our workbook, and I'll have a link at the end of the presentation for where you can download these handouts totally for free online in case you may share them with your patients.
Stage 1: First Change
In stage one, we certainly ask patients to make rapid changes. That's the expectation from day one. For patients who need to gain weight, we're asking them to start adding 500 calories a day this week from the very first session. And for patients who don't need to gain weight, we're assigning tasks that are based on their ARFID presentation. So for those who have sensory sensitivity, we might want them to make a small change in their preferred foods. So maybe if they will eat a certain flavor of chips, like nacho chips, then maybe we'll ask them to what about sour cream and onion chips, or jalapeno chips, just making some changes like that. We might ask them to reintroduce previously dropped foods.
Maybe they'll say, "Oh, I used to eat strawberries but I haven't done that for a year or two." We might say, "Well, why don't you go ahead and try to do some strawberries this week." We might have them rotate their preferred meals. So if they have exactly the same foods for breakfast, same for lunch, same for dinner every day, we might say, "Well, try to have your dinner for lunch or your lunch for dinner," just to kind of switch it up. And then for folks who have that fear of aversive consequences, we might ask them to already eliminate a minor safety behavior. For a patient who only wants to eat food in their own kitchen, we may ask them, why don't you eat it in another room, just to kind of start moving away from only having those certain safe cues.