How to Treat Patients with ARFID via Telehealth
Abridged transcript and slides
Presented by Dr. Jennifer Thomas (Massachusetts General Hospital) and Elissa Martinez LMFT (Recovery Record)
Access to the full webinar recording and all the slides are availabel from IAEDP.
Pages: 1 2 3 4 5 6 7 8 9 10 11
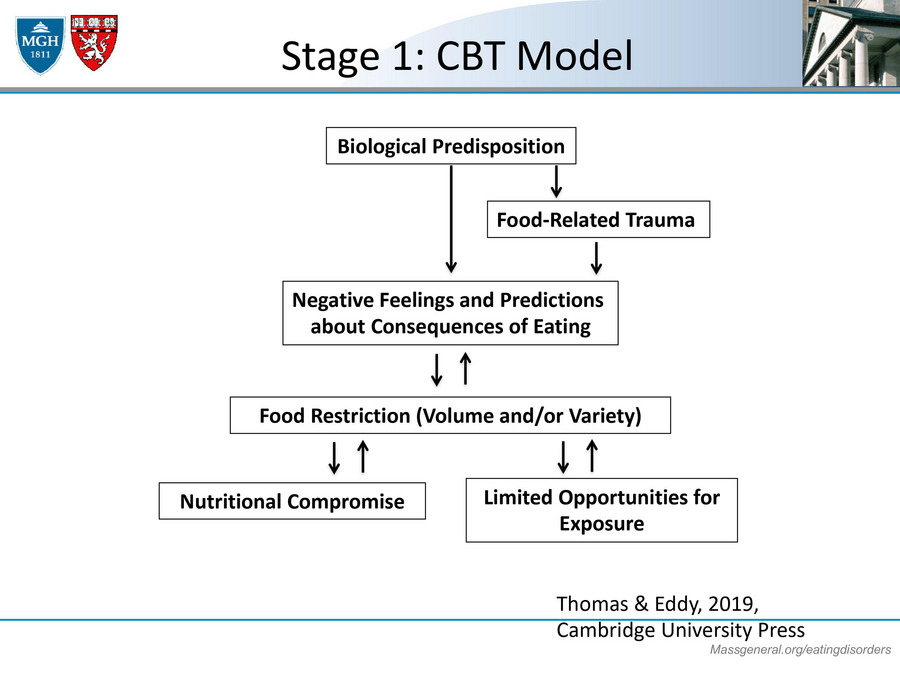
State 1: CBT Model
And then we also work with them to create a cognitive behavioral model of their ARFID. The way that we understand our food working is that first we think there is a biological predisposition either towards high anxiety or sensory, really things tasting very intense or basically having that low ghrelin level where they're not feeling hungry. And then in the setting of that predisposition, sometimes there's a trauma that's happened around choking or vomiting, like the patient I shared with you earlier who choked on the pork chop. And that regardless of what was the trauma or what is the predisposition, these patients start to develop negative feelings and predictions about the consequences of eating.
So they start to think, "Well, if I choked on that one pork chop, definitely I'll choke on meat. Probably I'll choke on any food that I eat and it's probably safer if I don't eat really at all to prevent myself from choking." Or they might think, "Well, wow, that one time that I tried kale, it was super disgusting. So I probably just shouldn't try any vegetables at all because I'll hate all of them." And so in the setting of those negative feelings and predictions, it totally makes sense that they would start restricting their food either by not eating enough volume or not eating enough variety.
The problem though is that then that food restriction leads to nutritional compromise. So they start to develop deficiencies. They start to get to be at a low weight potentially, or some of them might develop a higher weight that might be higher than what might be healthy for them. And certainly the food restriction can also lead to limited opportunities for exposure. So if you become known in your family as the person that won't eat at the table or won't eat foods with the family, they might stop asking you to participate in that. And so then you have fewer opportunities to eat with other people and to be exposed to new foods, which then circles back up to increasing the food restriction as well. So it becomes kind of a vicious cycle.
Now, in in-person treatment, we would probably draw out this formulation for the patient using their own words to try to piece it together, but in this virtual world my next telehealth tip is that often we'll use a screenshare to try to draw the formulation together either using PowerPoint or if that's a little too high tech for some folks, you can always draw it on a piece of paper and then hold up the piece of paper to the screen.
Stage 1: Therapeutics Meal (underweight patients only)
And then the last piece I'll say about stage one is that we do have a therapeutic meal for patients who are underweight. We try to invite them to bring a meal that comprises energy dense foods that are preferred foods. So kind of their favorite foods, things that are easy for them to eat. Oftentimes for patients with ARFID, that might be like Mac and cheese or chicken fingers or pizza. And then we also ask them to bring one novel food item. We coach either the parents in the family supported version or the patient themselves if this is individual. We give them specific instructions on how to increase volume and we pull a lot of these awesome ideas from family-based treatment for anorexia nervosa or FBT. We'll encourage them to increase their eating speed. Don't put down your fork, make specific requests, take another bite. Really persistence with a reasonable demand, "I know you can do it," and giving specific praise. And after the patient has eaten adequate volume in this meal, we'll encourage them to have one bite of their novel food item and try to provide that.
And my telehealth here is that during the family meal, it's great if you can have the family put the device or the patient put the device right at the kitchen table. I actually love doing family meals virtually because I think that it's almost better in a way. That it's a little artificial sometimes people come into the clinic to do these therapeutic meals but if you can almost feel like you're at the table with them, you get so much great information in telehealth.
CBT-AR Stage 2
Then after stage one, we move on to stage two. The main purpose of stage two is kind of a treatment planning type of foods. Here we provide psycho-education about the five basic food groups of fruits, vegetables, protein, grains, and dairy, as well as nutrition deficiencies that are common in folks with ARFID. And then we also help them select new foods to learn about in stage three and kind of think about what exposures they really want to focus on at that time.